Knockout Cell Line
Knockout Cell Line
Gene knockout technology can accurately remove or inactivate the specific genes. Constructing the gene knockout cell models is with wide applications in revealing the functions of genes in organisms and in scientific research, drug target screening, and other fields. The existing gene editing tools include CRISPR/Cas9, TALENs, or ZFNs. At present, the CRISPR/Cas9 system has become the preferred tool for gene knockout due to its high efficiency and ease of operation. This system utilizes the complementary gRNA to guide Cas9 nuclease to specifically recognize and cleave the target DNA, resulting in DNA double strand breaks (DSBs) and achieving gene knockout.
Service Details
| Cell Types | Various cell types, including tumor, conventional, stem, primary, and immortalized cell lines. |
|---|---|
| Services | Single-gene knockout / multi-genes knockout |
| Deliverables | Homozygous KO cell clones: ≥1 clone (2 vials per clone, 1 × 10^6 cells per vial) |
| Turnaround / Price |
As fast as 4 weeks |
EDI-Service Advantages
Efficient guide RNA Design
High-Performance Cas9 Protein
Efficient Cell Transfection
Streamlined Cell Screening Solutions
Knockout Cell Line Services
| Frameshift Mutation | guide RNA is targeted to an exon and the number of deletion bases is not a multiple of three. After knockout, a code-shifting mutation would cause gene knockout. |
|---|---|
| Large Fragment Deletion | Strategic guide RNA design to enable the deletion of substantial gene segments. |
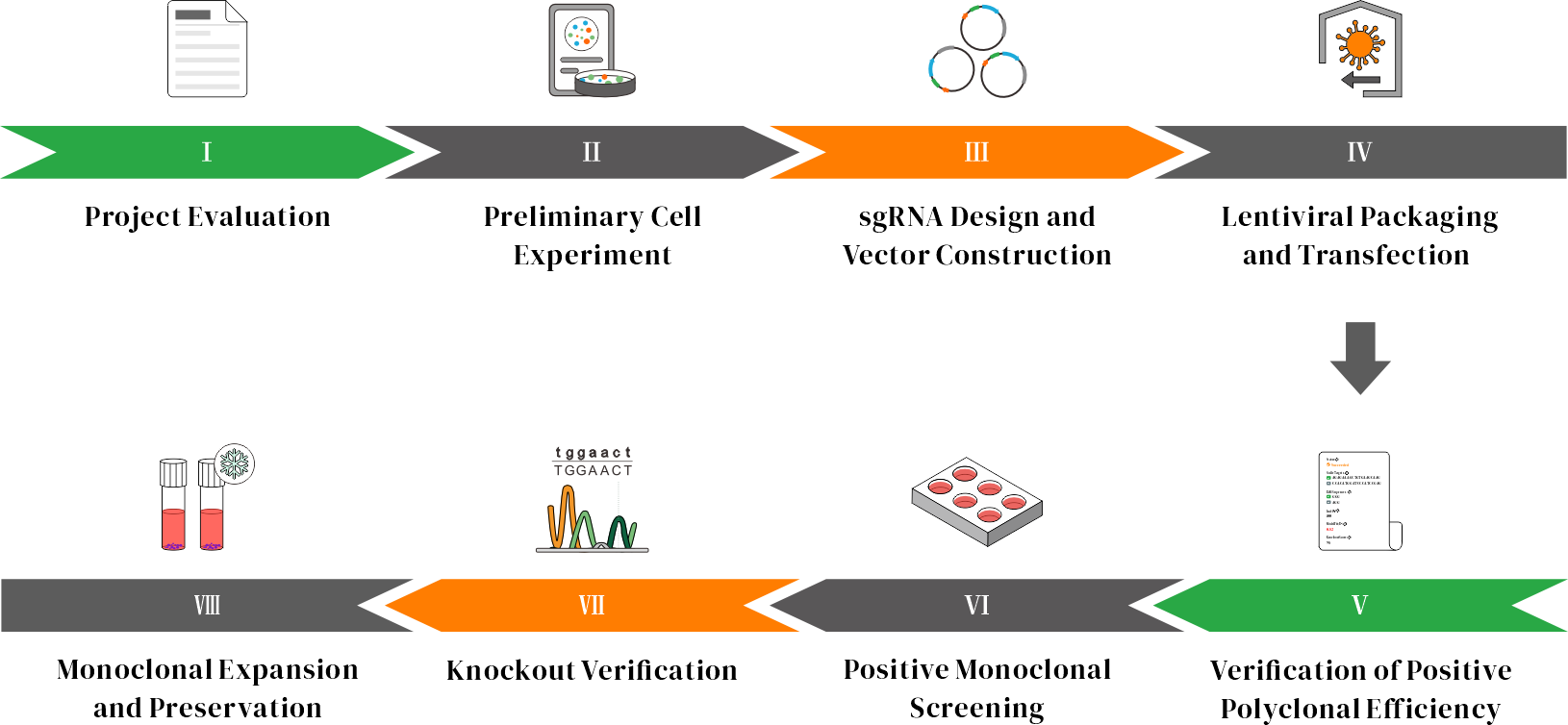
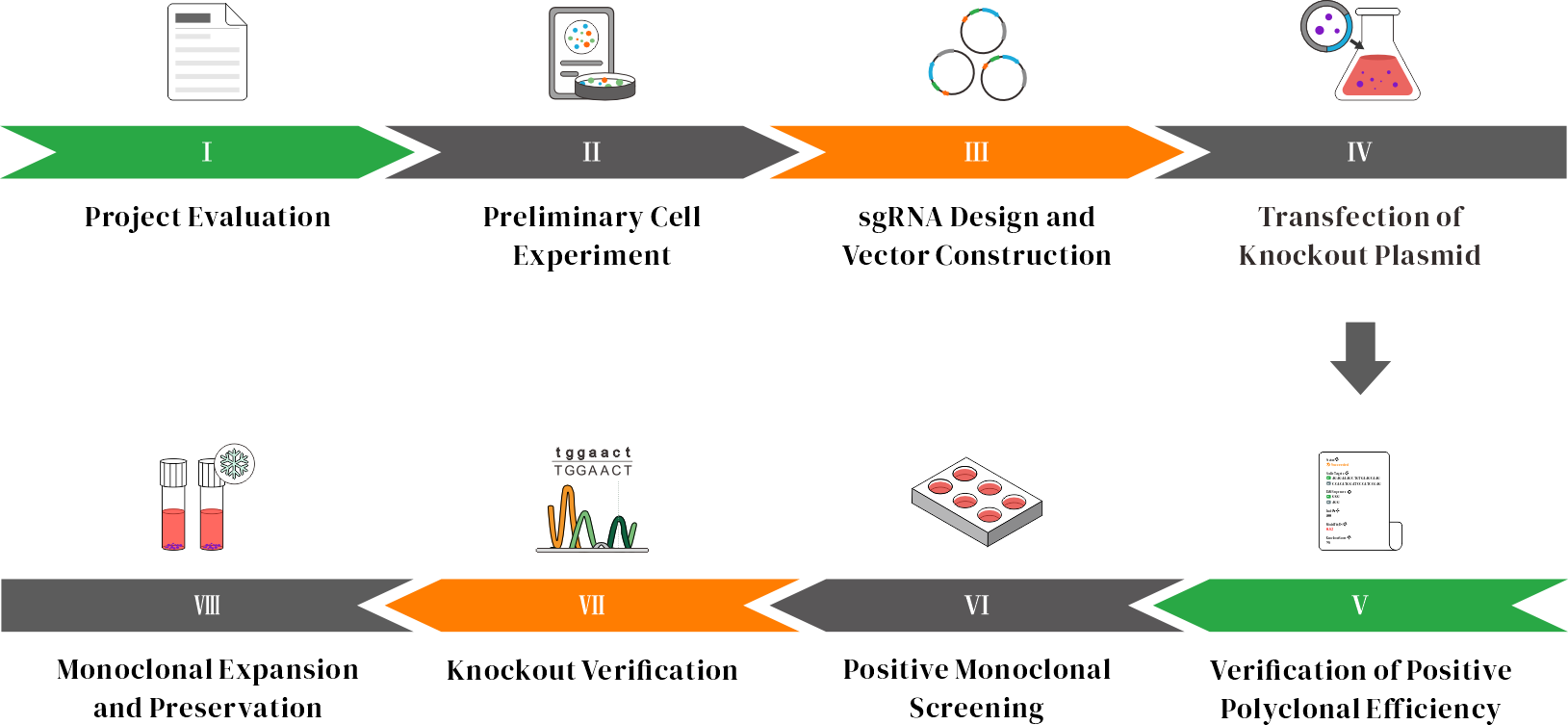
Workflow
Case Study
Objective: Single-Gene Knockout in HEK293 Cells
Project Goal: Achieved efficient knockout of Gene A in HEK293 cell lines, providing a robust model for downstream functional studies.
Project Design: sgRNA was designed in exon 2 of gene A.
Objective: Precise Small Fragment Knockout in Huh6 Cells
Project Goal: Successfully generated a small fragment deletion in Gene A within Huh6 cells, resulting in complete loss of target gene function.
Project Design: In Huh6 cells, two guide RNAs were designed to target the coding region of Gene A, achieving a fragment knockout.
Objective: Double Gene Knockout in THP-1 Cells
Project Goal: Engineered a simultaneous knockout of Gene B and Gene C in THP-1 cells, enabling the study of genetic interactions and compensatory mechanisms.
Project Design: Two sgRNAs were designed in the exon region of gene B, and two sgRNAs were designed in the exon region of gene C.
Advantage and Characteristic

Optimazied Strategy

Optimazied Strategy

Optimazied Strategy

Optimazied Strategy
Reference Materials
BRD4 gene knockout in skin squamous cell carcinoma (SCC) cells
Recent studies show that the incidence of skin squamous cell carcinoma (SCC) is rapidly increasing, with this and other non-melanoma skin cancers leading to numerous deaths annually. Over 20% of the global population may develop skin cancer during their lifetime. BRD4 has been proposed as a potential oncogenic protein, but its role in skin SCC remains understudied.
Researchers used CRISPR/Cas9 to directly knockout the BRD4 gene in SCC cells. BRD4-knockout or silenced cells showed a significant reduction in proliferation, and the expression of oncogenes closely related to cell proliferation (e.g., cyclin D1, Bcl-2, MYC) was significantly decreased. In vivo experiments showed that BRD4 knockout significantly inhibited tumor growth in A431 cells in SCID mice. BRD4 knockout cells and its relevant findings suggest that BRD4 could be a therapeutic target in skin squamous cell carcinoma.
FGFR1 gene knockout in MDA-MB-231 breast cancer cell line
The fibroblast growth factor (FGF)-fibroblast growth factor receptor (FGFR) signaling axis is a key mediator of interactions between the tumor stroma and cancer cells. FGFR1 activation through translocation, point mutations, or gene amplification can lead to cancer progression. In addition, G-protein-coupled estrogen receptor (GPER, GPR30) has been identified as a receptor mediating estrogen's role in various pathophysiological conditions.
To investigate how GPER mediates communication between cancer-associated fibroblasts (CAFs) and breast cancer cells through the FGF2/FGFR1 signaling axis, researchers used CRISPR/Cas9 gene editing to knockout FGFR1 in the MDA-MB-231 breast cancer cell line. Conditioned media (CM) from estrogen-stimulated CAFs induced the expression of connective tissue growth factor (CTGF) in FGFR1 wild-type (WT) MDA-MB-231 cells and promoted migration and invasion via the FGFR1-ERK1/2-AKT signaling pathway. However, this effect was significantly reduced or abolished in FGFR1-knockout cells. FGFR1 knockout cells have revealed a novel role of GPER in regulating FGF2 expression within the tumor microenvironment. The study confirmed that FGFR1 gene amplification is closely associated with overall survival rates in breast cancer patients, suggesting that FGFR1 could serve as a potential therapeutic target in breast cancer treatment. Furthermore, it elucidates the paracrine activation between cancer-associated fibroblasts (CAFs) and breast cancer cells, providing a theoretical foundation for the development of new therapeutic strategies.
BRCA1 gene knockout in Swan71 cell line
In early placental development, tumor suppressor genes and oncogenes work together to regulate cell proliferation and differentiation. BRCA1 is a well-known tumor suppressor gene that forms a complex with ZNF350 and CtIP to bind to the promoter region of the HMGA2 gene, preventing its transcription. This regulation has been studied in cancer cells but less so in placental cells.
Researchers used the CRISPR-Cas9 system to knockout the BRCA1 gene in the Swan71 cell line, generating BRCA1-knockout cells. Lentiviral particles with miR-182 overexpression were used to overexpress miR-182 in Swan71 cells. The results showed that BRCA1-knockout cells had significantly higher HMGA2 mRNA and protein levels compared to wild-type cells. miR-182 overexpression led to a decrease in BRCA1 protein levels and an increase in HMGA2 protein levels. BRCA Knockout Cell Lines and its relevant findings demonstrate that BRCA1 plays an important role in regulating HMGA2 levels in trophoblast cells and may be involved in placental development and function by influencing apoptosis, providing new insights into BRCA1's role in placental development.
ATM gene knockout in NGP and CHP-134 NB cell lines
Neuroblastoma (NB) is a common pediatric solid tumor characterized by high clinical and prognostic heterogeneity. Despite multiple treatment strategies, tumors in high-risk NB patients exhibit resistance to standard therapies and may progress to metastasis. ATM gene is involved in DNA damage response, and heterozygous deletions or hemizygous mutations of the ATM gene located on chromosome 11q are mutually exclusive in NB tumors. While ATM knockdown has been shown to promote tumor formation in NB cell lines in vitro and in vivo, the connection between ATM and tumor formation or cancer invasiveness remains unclear.
Researchers used CRISPR/Cas9 technology to knockout the ATM gene in NGP and CHP-134 NB cell lines, analyzing cell proliferation and colony formation capabilities, and protein expression related to DNA repair pathways through Western blot. In ATM-knockout cells, stable transfection of FANCD2 expression plasmids was used to overexpress FANCD2. Immunofluorescence microscopy was employed to determine protein expression. The results showed that ATM depletion leads to a decrease in FANCD2 protein levels, and ATM-knockout cells are more sensitive to the PARP inhibitor. Reintroduction of FANCD2 in ATM-knockout cells restored cell proliferation capacity. ATM knockout cells and its relevant findings reveal the role of ATM haploinsufficiency in neuroblastoma and illustrate how ATM inactivation enhances NB cell sensitivity to PARP inhibitor, which is significant for treating high-risk NB patients with ATM gene dosage and cancer progression issues.
Selected Customer Resources
Deep whole-genome analysis of 494 hepatocellular carcinomas
Abstract:
To date, more than half of global hepatocellular carcinoma (HCC) cases occur in China, yet comprehensive whole-genome analyses focusing on HBV-related HCC within the Chinese population remain scarce. To address this challenge, researchers initiated the China Liver Cancer Atlas (CLCA) project, aiming to conduct large-scale whole-genome sequencing to unravel the unique pathogenic mechanisms and evolutionary trajectories of HCC in China.
The researchers performed deep whole-genome sequencing on 494 HCC tumor samples, with an average depth of 120×, alongside matched blood controls, providing a detailed genomic landscape of HBV-associated HCC. Beyond confirming well-known coding driver genes such as TP53 and CTNNB1, the study identified six novel coding drivers—including FGA—and 31 non-coding driver genes.
Additionally, the research uncovered five new mutational signatures, including SBS_H8, and characterized the presence of extrachromosomal circular DNA (ecDNA) formed via HBV integration, which contributes to oncogene amplification and overexpression. Functional validation experiments demonstrated that mutations in genes such as FGA, PPP1R12B, and KCNJ12 significantly enhance HCC cell proliferation, migration, and invasion.
These findings not only deepen our insights into the genomics of HCC, but also open up new potential targets for diagnosis and therapy. View details>>
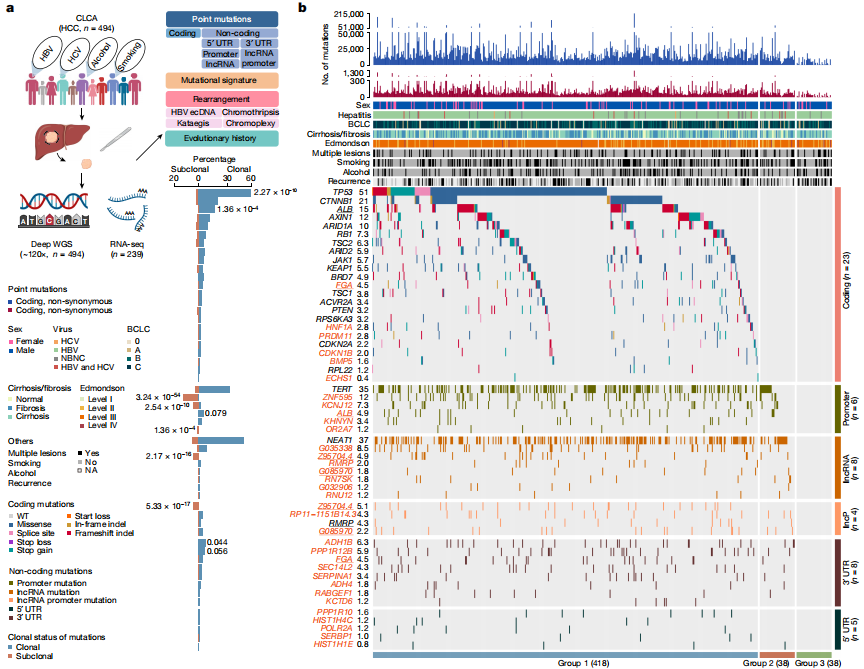
Candidate driver landscape
Targeted Macrophage CRISPR-Cas13 mRNA Editing in Immunotherapy for Tendon Injury
Abstract:
During the acute inflammatory phase of tendon injury, excessive activation of macrophages leads to the overexpression of SPP1, which encodes osteopontin (OPN), thereby impairing tissue regeneration. The CRISPR-Cas13 system holds great promise for tissue repair due to its unique RNA editing and rapid degradation capabilities; however, its application has been limited by the lack of efficient delivery methods.
To address this, the researchers systematically screened various cationic polymers targeting macrophages and developed a nanocluster carrier capable of efficiently delivering Cas13 ribonucleoprotein complexes (Cas13 RNPs) into macrophages. Utilizing a reactive oxygen species (ROS)-responsive release mechanism, this system specifically suppresses the overexpression of SPP1 in macrophages within the acute inflammatory microenvironment of tendon injury.
Experimental results demonstrated that this targeted delivery strategy significantly reduced the population of SPP1-overexpressing macrophages induced by injury, inhibited fibroblast activation, and alleviated peritendinous adhesion formation. Furthermore, the study elucidated that SPP1 promotes fibroblast activation and migration through the CD44/AKT signaling pathway, and that inhibiting this pathway effectively mitigates adhesion formation following tendon injury. View details>>
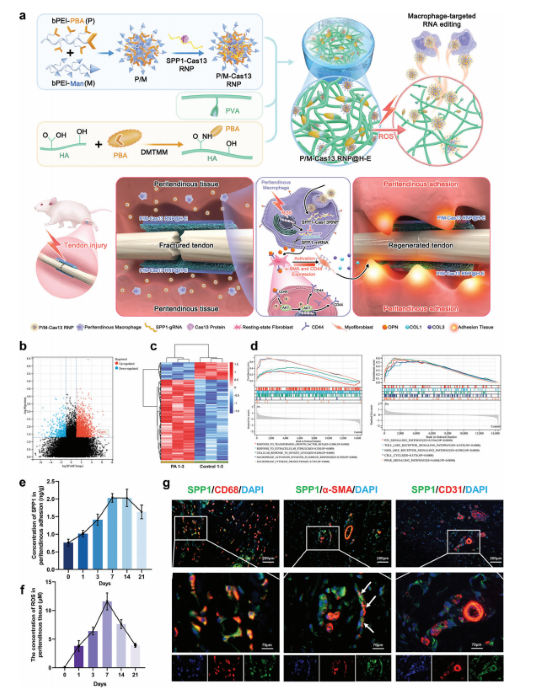
Schematic diagram illustrating immune microenvironment-activated mRNA editing strategies of macrophages for PA therapy
Electrical stimulation of piezoelectric BaTiO3 coated Ti6Al4V scaffolds promotes anti-inflammatory polarization of macrophage and bone repair via MAPK/JNK inhibition and OXPHOS activation
Abstract:
Spinal cord injury (SCI) is a severe disabling condition that causes permanent loss of sensory, autonomic, and motor functions. While stem cell therapies, particularly mesenchymal stem cells (MSCs), show great promise for SCI treatment, their limited regenerative capacity restricts their application in tissue repair. The researchers observed that extracellular vesicles derived from antler bud progenitor cells (EVsABPC) may carry bioactive signals that promote tissue regeneration. Accordingly, they isolated and engineered EVs from ABPCs for SCI therapeutic investigation.
The study found that EVsABPC significantly enhanced neural stem cell (NSC) proliferation, promoted axonal growth, reduced neuronal apoptosis, and modulated inflammation by shifting macrophage polarization from the pro-inflammatory M1 phenotype to the anti-inflammatory M2 phenotype. Moreover, engineered EVsABPC modified with cell-penetrating peptides demonstrated improved targeting to the SCI lesion site, markedly enhancing neural regeneration and functional motor recovery. These findings highlight EVsABPC as a promising candidate for SCI therapy. View details>>
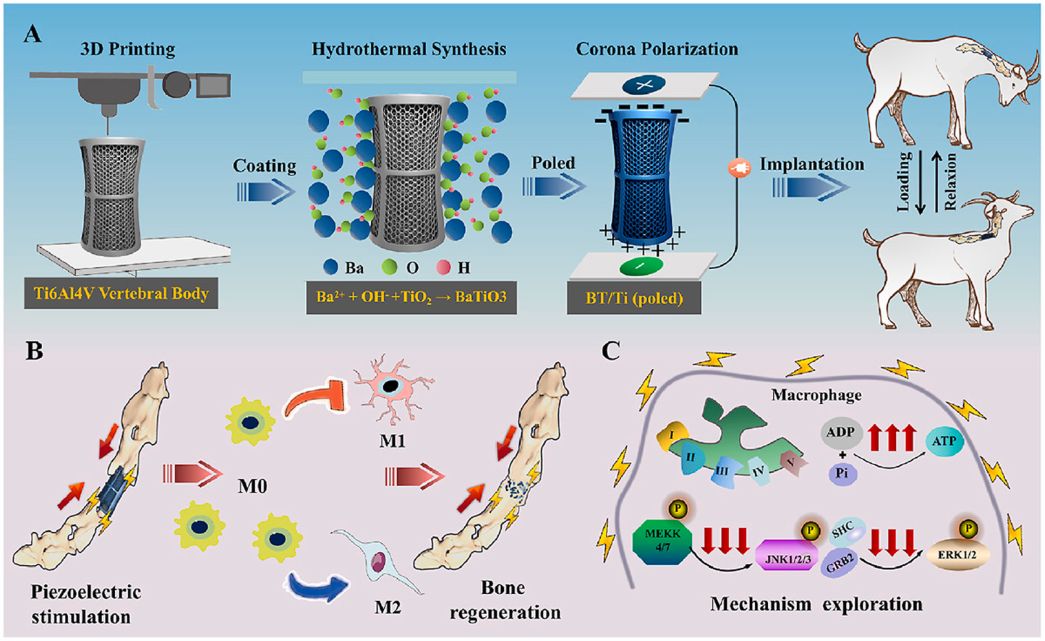
Graphical abstract
Generation of recombinant antibodies by mammalian expression system for detecting S-metolachlor in environmental waters
Abstract:
S-metolachlor (S-MET) is one of the most widely produced and applied herbicides in China. Owing to its chemical properties, it tends to persist in soil and easily contaminates surface and groundwater through leaching and runoff. This environmental persistence poses a serious threat to plant development and, through the food chain, to human health.
To address the limitations of current detection technologies and meet the growing demand for high-efficiency analytical tools, the researchers employed a mammalian expression system to generate recombinant antibodies targeting S-MET.
Building on the successful expression of these antibodies, they established a sensitive immunoassay for monitoring S-MET residues in various environmental water samples. The icELISA results showed that the recombinant antibodies retained the sensitivity, specificity, and biological activity of the original monoclonal antibodies, delivering accurate and reproducible detection in river water, agricultural runoff, and tap water. View details>>
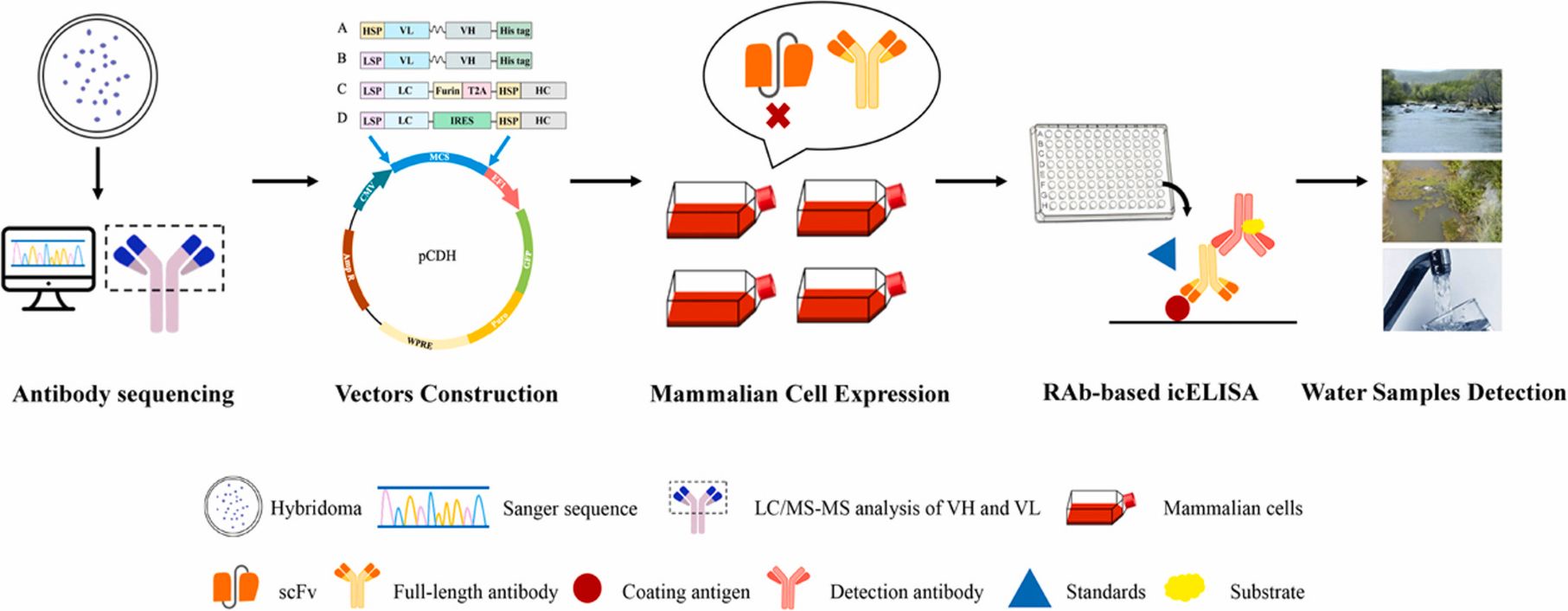
Graphical abstract
Dumbbell probe initiated multi-rolling circle amplification assisted CRISPR/Cas12a for highly sensitive detection of clinical microRNA
Abstract:
MicroRNAs (miRNAs) are a class of small non-coding RNA molecules that regulate gene expression by interacting with the mRNAs of target genes. Given their crucial role in the development and progression of various diseases, miRNAs have emerged as promising biomarkers for clinical diagnostics.
In this study, researchers established a novel detection platform, termed DBmRCA, which combines dumbbell probe-initiated multi-rolling circle amplification with the high-sensitivity signal output of CRISPR/Cas12a. This enzyme-free, isothermal method enables accurate quantification of miRNA within just 30 minutes.
Clinical validation revealed that the expression levels of miR-200a and miR-126 were significantly downregulated in lung cancer tissues, and results from DBmRCA were consistent with those obtained by conventional techniques. With its high sensitivity, rapid turnaround, and simplified workflow, the DBmRCA platform presents a reliable tool for miRNA detection and holds strong promise for early diagnosis and therapeutic monitoring of lung cancer. View details>>
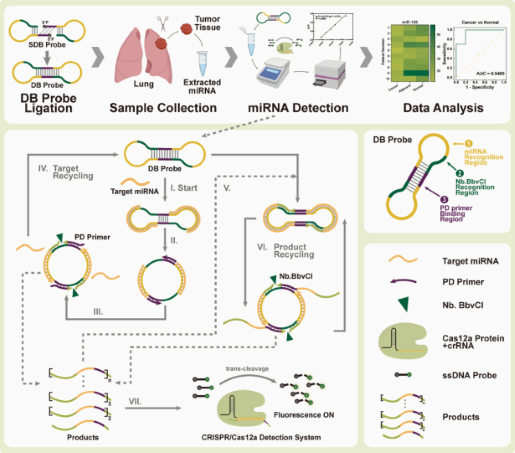
Graphical abstract